Speech pathologists: let’s improve our progress notes to help our clients – and ourselves
Why it matters:
Writing good file/progress notes of our consultations is:
- required by our Professional Standards, Code of Ethics, Statutory Code of Conduct and NDIS Code of Conduct; and
- helpful if a complaint is made against us or if we are sued, e.g., for professional negligence.
Case in point:
D Lane v Northern NSW Local Health District [2013] NSWDC 12
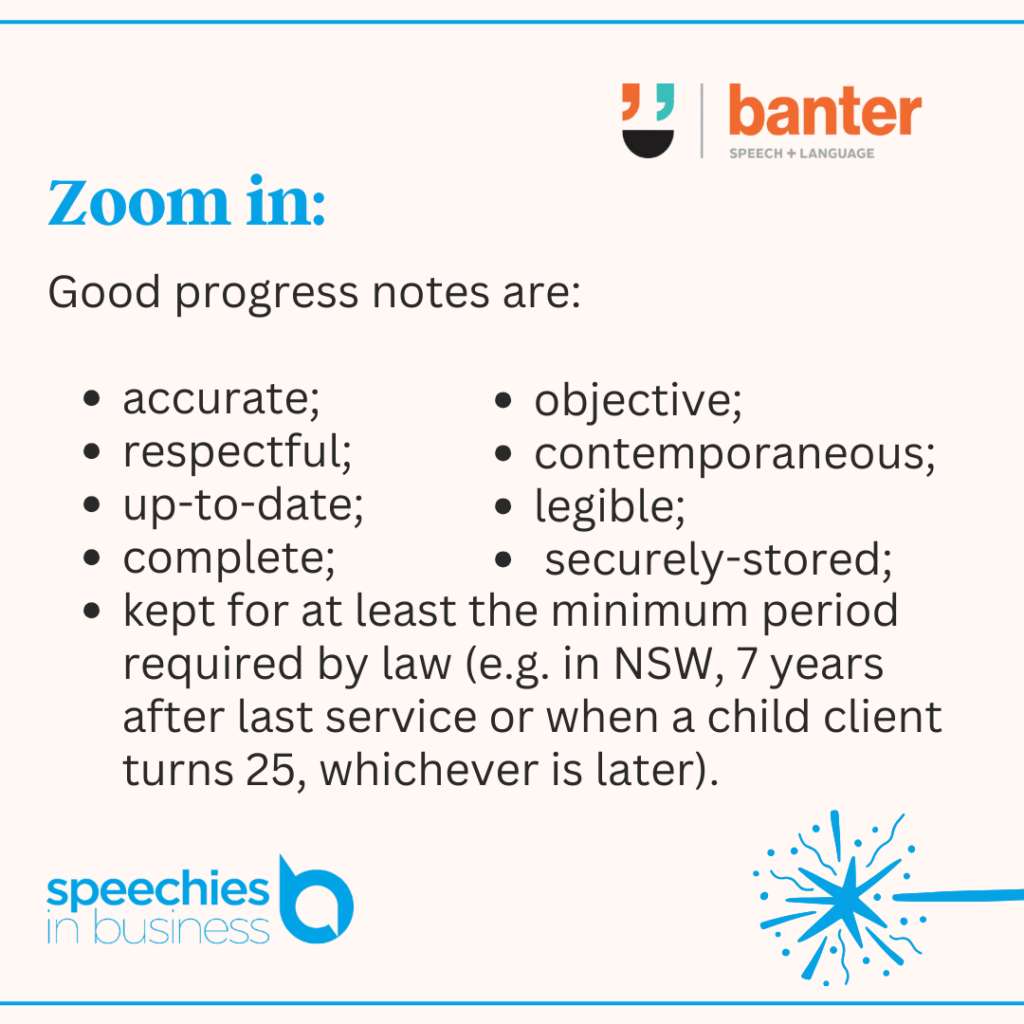
Zoom in:
Good progress notes are:
- accurate;
- objective;
- respectful;
- contemporaneous;
- up-to-date;
- legible;
- complete;
- securely-stored; and
- kept for at least the minimum period required by law (e.g. in NSW, 7 years after last service or when a child client turns 25, whichever is later).
Yes, but:
Good note taking takes time and energy. You need a system to ensure progress note-taking fits into your daily workflows and doesn’t get on top of you.
Go deeper:
To read more about our progress note system, check it out here.
Read more:
D Lane v Northern NSW Local Health District [2013] NSWDC 12
Australian SLPs: do you store progress notes in a cloud-based practice management system?