Interpersonal conflicts are common. They can make us worry and react in regrettable ways that make us feel bad about ourselves. Sometimes, we withdraw from relationships, which is also not good for us.
Conflict with people can lead to lots of bad outcomes: reduced focus and creativity, worse decision making, and unhappy relationships.
None of us is perfect when it comes to relationships. When you are in conflict with someone else, there are several strategies you can use to find a healthy way forward:
- Remember your perspective is just one amongst many. Sometimes, we forget that we all have different viewpoints and values and think that our view is correct and all other views are uninformed, irrational or biased. Thus is not always true – not everyone sees things that same way and that’s okay.
- Be aware everyone is biased (including you!). We sometimes assume that other people’s behaviour is due to their personality, when it might just be due to their situation. Ask someone you trust to help you reflect on the ways you might be seeing the situation unfairly.
- Avoid black and white thinking. Sometimes, when we disagree with others, we start to think that the other person is an opponent or even enemy! Rather than thinking it’s ‘you versus them’, focus on the decision or situation instead and try to make progress on it. Think of yourself and the other person as sitting on opposite sides of a seesaw and work together to find a balance.
- Know your goals: Avoid drama and stay focused on your goals, e.g. you want a healthy relationship that will last into the future, and you want to feel less angry/frustrated after interactions. Make a list of your goals and circle the most important ones. You don’t need to be best friends with the other person – focus first on having a functional, respectful relationship.
- Don’t gossip or look for drama: It’s perfectly fine to seek help with sorting out your feelings and to check in with others. But choose who you speak with carefully and look for people who are constructive and who will challenge your perspective – people who will help you solve the specific problem.
- Experiment: There is no one way to solve interpersonal conflicts. Your strategy will depend on the situation and the people involved. Experiment and see what happens: e.g. decide that for two weeks you will listen to the other person, and not interrupt, and focus on what they are saying (rather than how they say it). Try to summarise what the other person is saying, and check you have understood them. Try to interrupt your conflict patterns of the past.
- Stay curious: People are complex! Try to learn more about the other person. Do not approach conversations with aggression or defensiveness, but with creativity and with genuine questions about them. Think about a future when you have overcome the conflict.
- Don’t give up: With good faith efforts and hard work, you can resolve most interpersonal conflicts.
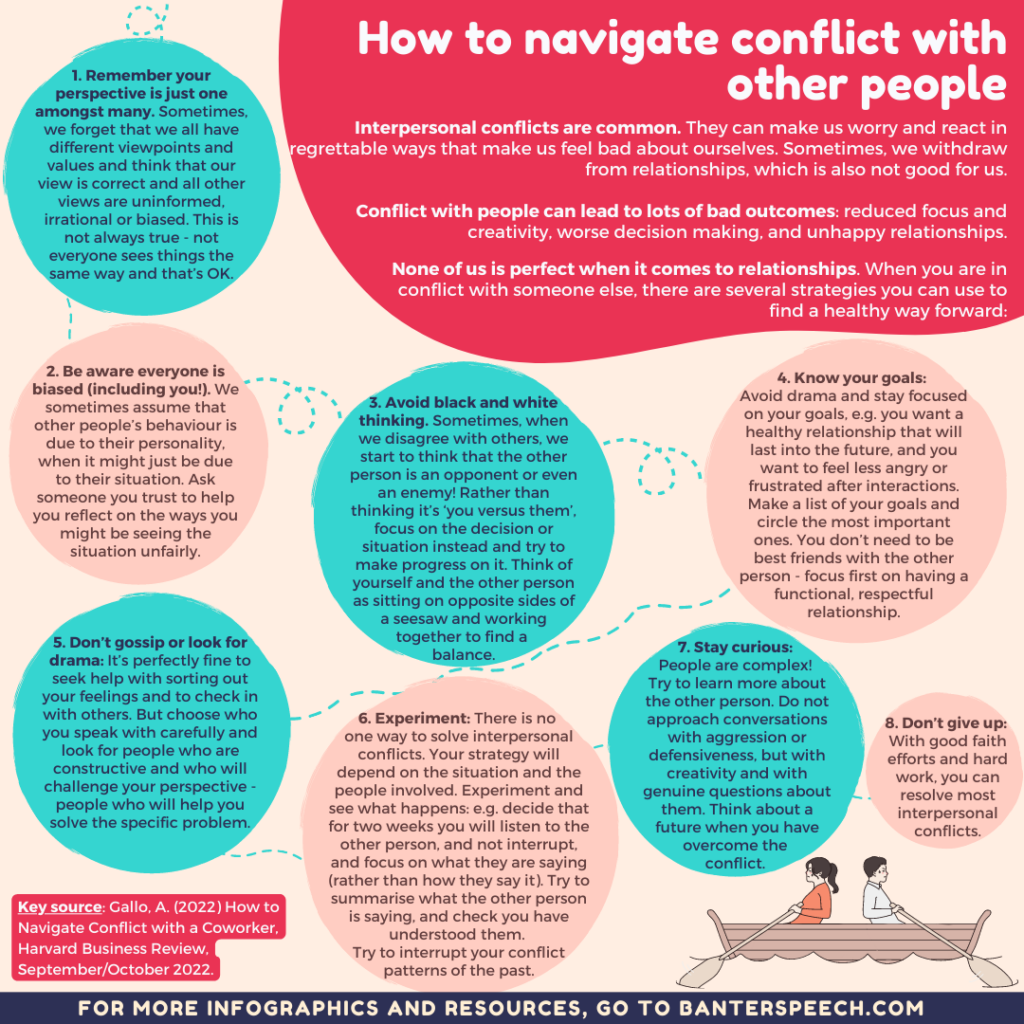
Key source: Gallo, A. (2022) How to Navigate Conflict with a Coworker, Harvard Business Review, September/October.
For more on supervision, check out our book “How to supervise speech pathologists properly in private practice“.
This infographic also appears in a recent issue of Banter Booster, our weekly round up of the best speech pathology ideas and practice tips for busy speech pathologists, speech pathology students, and other interested readers.
Sign up to receive Banter Booster in your inbox each week: